In October 2018, the National Secular Society and the Secular Medical Forum held a joint conference on Healthcare and Secularism. The final two talks concerned assisted dying and the right to die. Both talks were excellent. Videos of the talks are available on YouTube and are embedded here with some description and comments.
1. Dr. Jacky Davis – An Update on Assisted Dying – One hundred million people now have access to it, why can’t we?
Jacky Davis is the Chair of Healthcare Professionals for Assisted Dying (HPAD). Jacky is also a consultant radiologist at Whittington Hospital; a member of the BMA Council and of the BMA ethics committee; and a board member of Dignity in Dying.
The talk makes many excellent points – especially in covering why it is so difficult for the BMA to change its approach on assisted dying. Policy is decided by an annual conference of only 300 people. The BMA have so far refused to hold a ballot of all their members on whether to adopt a neutral position on assisted dying. MDMD strongly endorse Jacky’s calls for the BMA to hold such a vote.
Of particular interest to MDMD is Jacky’s description of a public debate in Gloucester which she took part in prior to the 2015 Marris Bill debate in the House of Commons. She said “I was in a position I often find myself in. I was being attacked because they [the audience] didn’t think that our position on assisted dying went far enough.”
Jacky went on to discuss criticism of the 6 month criterion. She dismissed, as “another straw man”, the argument used by some, that the difficulty of accurate prognosis was a reason for not changing the law. She then described those who wish to be able to have a medically assisted death: “These people are not people who want to commit suicide. These are people who want to live as long as they can, until they don’t want to any more.”
One really positive suggestion Jacky put forward was with the practicalities of doctors working with an assisted dying law. She estimated that, extrapolating from the situation in Oregon, each GP practice would expect to see one patient who wanted as assisted death every 7 years. GPs might reasonably be concerned that they wouldn’t know how to deal with such rare events. Jacky suggested regional teams of trained experts who GPs could work with.
2. Dr Michael Irwin – When will MARS (Medically Assisted Rational Suicide) land on the UK?
Michael was Medical Director of the United Nations; chairman of the Voluntary Euthanasia Society prior to it changing its name to “Dignity in Dying”; and a past president of the World Federation of Right-to-Die Societies. He founded the Society for Old Age Rational Suicide in 2009 and was its coordinator until 2015, after which it was renamed “My Death, My Decision” (MDMD). Michael is a patron of MDMD.
Michael picked up on a number of points made by Jacky, saying “I’m very much is favour of the Oregon Bill, but as a start, it should go much further.”
Michael discussed some different approaches to defining “terminal illness”, contrasting a GMC reference to “dying over the next 12 months” to the Oregon Bill’s 6 months, and the situation in Scotland where a recent change to benefit legislation replaced a 6 month “terminal illness” criterion with an evaluation by doctors on a case by case basis without requiring an estimate of life expectancy.
Michael pointed out that there is currently uneasiness in Oregon over their 6 month criterion with moves to expand it to cover longer term degenerative diseases.
MDMD Conclusions
These are two very experienced campaigners, both with a strong medical background. It is fascinating to hear both the common ground and the differences in their views. From MDMD’s perspective Jacky’s defence of the 6 month criterion does not stand up to serious scrutiny, although it may be a realistic political compromise in the UK and elsewhere in the short or medium term. We recognise that is has provided an important option to millions of people around the world – which we in the UK do not have.
However, dismissing the difficulties of accurately giving a life expectancy prognosis as a “straw man” seems too simplistic. Even without the moral dilemma of assisted dying, Scottish doctors found the criterion unacceptable and successfully pressed for this to be removed as a criterion in benefit assessments. If this is the case for benefit assessment, why not also for assisted dying?
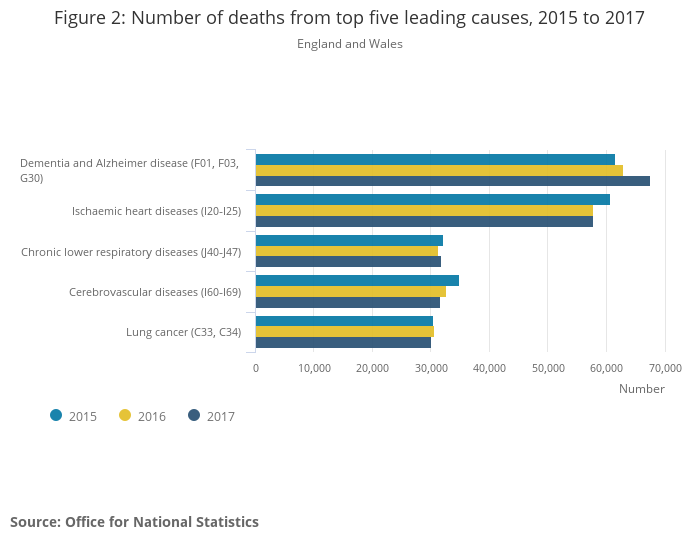
Even more importantly, MDMD fully agrees with Jacky’s statement that the people who should be allowed access to medical assistance to die are “… people who want to live as long as they can, until they don’t want to any more”, (when this is due to the intolerable and incurable medical conditions they face, which even the best palliative care cannot alleviate). But Jacky’s description includes high profile cases like Tony Nicklinson, Debbie Purdy, and Omid T. None of these people could be helped by the Oregon-style law she advocates. In addition, some of those in early stage dementia fit her description, while they retain mental capacity – people like Alex Pandolfo who plans to go to Switzerland to end his life when his condition becomes unbearable for him. They face the later stages of dementia when mental capacity will be lost, but are also ineligible for help from an Oregon-style law. Dementia is now the cause of 1 in 8 of all deaths in England and Wales – and nearly 1 in 4 deaths of women over 80, according to the latest ONS data.
In her final interview, in December 2014, Debbie Purdy, who worked closely with Dignity in Dying in her campaign work, said “I think Lord Falconer, in saying that if you’re within the last six months of your life, misses the point that Tony Nicklinson, myself, Paul Lamb – the people whose cases have all been public – all have to face decades of a life that we don’t consider acceptable, and that is the thing I find hardest.” Michael Irwin, together with MDMD, Friends at the End and Humanists UK, very clearly support Debbie’s point of view. Jacky Davis failed to explain why she advocates an approach which wouldn’t help people like Debbie, while at the same time arguing for “people who want to live as long as they can, until they don’t want to any more”, to have the option of a medically assisted death, which is just what Debbie wanted. With this approach, we expect that Jacky will continue to hear the views she described from her audience in Gloucester.
The post Videos from Healthcare and Secularism 2018 Conference appeared first on My Death, My Decision.



 ds Legislative Assembly has
ds Legislative Assembly has